CROSS-REFERENCES TO RELATED APPLICATIONS
[0001] This application claims the benefit of U.S. Provisional Application No. 60/780,692, filed 9 Mar. 2006, and U.S. Provisional Application No. 60/777,682, filed 28 Feb. 2006. The contents of these applications are incorporated by reference.
STATEMENT REGARDING FEDERALLY SPONSORED RESEARCH
[0002] The U.S. government may own rights in this invention pursuant to grant numbers A150564 and A157156 from the National Institutes of Health/NIAID.
BACKGROUND OF THE INVENTION
[0003] A. Field of the Invention
[0004] The present invention concerns attenuated Francisella bacteria vaccines and methods of preventing and treating a Francisella infection.
[0005] B. Background of the Invention
[0006]Francisella tularensis is an intracellular Gram negative bacterium that can cause pneumonic tularemia in humans (Ellis et al., 2002; Tarnvik, 1989). F. tularensis subsp. tularensis is classified as one of the most infectious pathogenic bacteria because inhalation with only a few organisms will cause disease and significant mortality (Saslaw et al., 1961). F. tularensis also is considered a potential biological weapon and has been developed as a germ warfare agent by several government programs (Christopher et al., 1997; Dennis et al., 2001; Harris, 1992). Humans infected by F. tularensis usually acquire the disease by contact with infected animals, vectors (ticks), exposure to contaminated food and water, or aerosol exposure (Feldman et al., 2001; Tarnvik, 1989).
[0007] To date, F. tularensis live vaccine strain (LVS), which is derived from F. tularensis subspecies holarctica (type B) has been the only vaccine candidate for tularemia. In humans (Saslaw et al., 1961) and in animals (Eigelsbach and Downs, 1961), vaccination with LVS has demonstrated varying degrees of protection against aerosolized and parenteral subsp. tularensis challenges. However, the basis of attenuation of the LVS strain is unknown, making its use in humans somewhat questionable given the uncertain probability of reversion to virulence of the vaccine strain.
SUMMARY OF THE INVENTION
[0008] The present invention overcomes the deficiencies in the art by providing compositions and methods for their use in live bacteria compositions. In certain aspects the live bacteria compositions contain attenuated bacteria for use in provoking an immune response to non-attenuated bacteria. Further aspects of the invention include vaccine comprising attenuated bacteria of the genus Franscisella, in particular the species Francisella tularensis. In still other aspects of the invention are directed to modified subspecies F. tularensis novicida, F. tularensis tularensis, or F. tularensis holarctica.
[0009] Embodiments of the invention include methods of inducing an immune response in a subject comprising administering to the subject a Francisella bacterium that includes an alteration in the nucleic acid sequence encoding the mglA, iglA, iglB, iglC, or iglD gene of the bacterium. In certain aspects the bacterium is attenuated. The alteration in the nucleic acid sequence can render the mglA, iglA, iglB, iglC, or iglD gene inactive. In one aspect the mglA gene is altered. In a second aspect the iglA gene is altered. In a third aspect the iglB gene is altered. In a fourth aspect the iglC gene is altered. In a fifth aspect the iglD gene is altered.
[0010] In a further embodiment the methods may include a bacterium with at least two, three, four, or five of the mglA, iglA, iglB, iglC, or iglD genes altered. In certain aspects all of the mglA, iglA, iglB, iglC, and iglD genes are altered. In other aspects one or more of the mglA, iglA, iglB, iglC, or iglD gene is not expressed. In still other aspects the bacterium lacks the mglA, iglA, iglB, iglC, or iglD gene. An alteration can be a deletion, substitution, or insertion mutation. In still further aspects of the invention the bacterium expresses an inactive mglA, iglA, iglB, iglC, or iglD protein. In certain aspects of the invention the bacterium is F. tularensis. The F. tularensis bacterium can be F. tularensis tularensis (Type A), F. tularensis holarctica (Type B), F. tularensis mediaasiatica, and F. tularensis novicida. In one aspect, F. tularensis is F. tularensis tularensis (Type A). In a second aspect, F. tularensis is F. tularensis holarctica (Type B). In a third aspect, F. tularensis is F. tularensis mediaasiatica. In a fourth aspect, F. tularensis is F. tularensis novicida. In a further aspect F. tularensis novicida is F. tularensis novicida strain KKF34 or KKF24. The bacterium of the invention can be comprised in a pharmaceutically acceptable composition. The composition can be formulated into a liquid, spray, or aerosol. The bacterium of the invention can be administered intravenously (e.g., by injection) or intranasally.
[0011] In yet another aspect the bacterium are incapable of replicating. In certain aspects bacterium is incapable of replicating in a cell. In a further aspect the bacterium is incapable of replicating in a macrophage or an amoebae. In a particular aspect the bacterium is incapable of replicating in an amoebae. In still a further aspect the bacterium is incapable of replicating in the subject. The subject can be an animal. The animal can be a human, mouse, rat, rabbit, cat, dog, pig, or cow. In particular aspects the animal is a human.
[0012] The methods of the invention may further include (a) producing a protective immune response in the subject; (b) preventing against or treating Francisella bacterial infection; (c) preventing against or treating pulmonary Francisella bacterial infection; (d) preventing a pulmonary challenge of Francisella bacterial infection; and/or (e) preventing or treating tularemia.
[0013] Methods of the invention include methods of preventing or treating Francisella bacterium infection comprising administering to a subject an attenuated Francisella bacterium that includes an alteration in the nucleic acid sequence encoding the mglA, iglA, iglB, iglC, or iglD gene of the bacterium.
[0014] Methods of the invention also include methods for producing an attenuated Francisella bacterium comprising introducing an alteration in the nucleic acid sequence encoding the mglA, iglA, iglB, iglC, or iglD gene of the bacterium. An alteration can include a deletion, substitution, or insertion mutation. In certain aspects one or more of the mglA, iglA, iglB, iglC, or iglD gene is not expressed. In other aspects of the invention the bacterium expresses one or more inactive mglA, iglA, iglB, iglC, or iglD protein. In still further aspects the bacterium lacks one or more of the mglA, iglA, iglB, iglC, or iglD gene. The bacterium or bacteria of the invention can be formulated into a pharmaceutically acceptable vaccine.
[0015] Further embodiments of the invention include methods of vaccination against a Francisella bacterium comprising administering to a subject an attenuated Francisella bacterium having a genome comprising an alteration in the nucleic acid sequence encoding one or more of the mglA, iglA, iglB, iglC, or iglD gene of the bacterium. The composition typically comprises a pharmaceutically acceptable formulation.
[0016] Still further embodiments of the invention include vaccine compositions comprising an attenuated Francisella bacterium with a genome that comprises an alteration in the nucleic acid sequence encoding the mglA, iglA, iglB, iglC, or iglD gene of the bacterium. Vaccine composition of the invention can comprise an adjuvant.
[0017] Yet still further embodiments of the invention include methods for inducing an immune response against a Francisella bacterium comprising administering to a subject an effective amount of a vaccine compositions described herein. The composition can be administered to the subject at least 2, 3, 4, 5, 6, 7, 8, 9, 10, or more times. In certain aspects of the invention an adjuvant is administered with the vaccine composition(s).
[0018] Embodiments of the invention include methods for producing a vaccine for a Francisella bacterial infection comprising generating or obtaining an attenuated Francisella bacterium that includes an alteration in the nucleic acid sequence encoding one or more of the mglA, iglA, iglB, iglC, or iglD gene of the bacterium and formulating a pharmaceutically acceptable composition comprising one or more bacterium encoding one or more altered genes.
[0019] Further embodiments of the invention include vaccine compositions comprising an immunologically protective amount of a first attenuated, non-reverting altered Francisella bacterium in which one or more of the mglA, iglA, iglB, iglC, or iglD gene has been inactivated.
[0020] Further embodiments of the invention include live attenuated vaccines for the protection of animals against infection with pathogenic Francisella, said live attenuated vaccine comprising: (a) a live attenuated Francisella bacterium that is incapable of expressing a functional mglA, iglA, iglB, iglC, or iglD protein, wherein the bacterium includes an alteration in the mglA, iglA, iglB, iglC, or iglD gene; and (b) an adjuvant. In certain aspects the bacterium can further comprise a heterologous gene. The vaccine will typically comprise sufficient attenuated Francisella bacteria to elicit an immune response in a subject.
[0021] Embodiments of the invention include methods of protecting a subject against infection with pathogenic Francisella bacteria comprising administering to the subject a live attenuated Francisella bacterium that is incapable of expressing a functional mglA, iglA, iglB, iglC, or iglD protein, wherein the bacterium includes an alteration in the mglA, iglA, iglB, iglC, or iglD gene.
[0022] The inventors also contemplates that equivalent genes (e.g., greater than 80% homology) in other gram negative bacteria can be similarly inactivated to provide efficacious vaccines.
[0023] “Inactivated” gene includes a gene that has been mutated by insertion, deletion or substitution, or a combination thereof of nucleotide sequence such that the mutation inhibits or abolishes expression and/or biological activity of the encoded gene product. The mutation may act through affecting transcription or translation of the gene or its mRNA, or the mutation may affect the polypeptide gene product itself in such a way as to render it inactive.
[0024] “Attenuated” includes a cell, culture, or strain of Francisella exhibiting a detectable reduction in infectivity or virulence in vitro or in vivo as compared to that of the parent strain of Francisella from which the attenuated cell, culture, or strain is derived. Reduction in virulence encompasses any detectable decrease in any attribute of virulence, including infectivity in vitro or in vivo, or any decrease in the severity or rate of progression of any clinical symptom or condition associated with infection.
[0025] In addition to immunizing the recipient, the vaccines of the invention may also promote growth of the recipient and/or boost the recipient's immunity and/or improve the recipient's overall health status.
[0026] The subject to be immunized may be a human or other mammal or animal, for example, farm animals including cows, sheep, pigs, horses, goats and poultry (e.g., chickens, turkeys, ducks and geese) and companion animals such as dogs and cats; exotic and/or zoo animals. Immunization of both rodents and non-rodent animals is contemplated.
[0027] It is contemplated that any embodiment discussed in this specification can be implemented with respect to any method or composition of the invention, and vice versa. Furthermore, compositions of the invention can be used to achieve methods of the invention.
[0028] The term “about” or “approximately” are defined as being close to as understood by one of ordinary skill in the art, and in one non-limiting embodiment the terms are defined to be within 10%, within 5%, within 1%, and within 0.5%.
[0029] The terms “inhibiting” or “reducing” or any variation of these terms, when used in the claims and/or the specification includes any measurable decrease or complete inhibition to achieve a desired result.
[0030] The term “effective,” as that term is used in the specification and/or claims, means adequate to accomplish a desired, expected, or intended result.
[0031] The use of the word “a” or “an” when used in conjunction with the term “comprising” in the claims and/or the specification may mean “one,” but it is also consistent with the meaning of “one or more,” “at least one,” and “one or more than one.”
[0032] The use of the term “or” in the claims is used to mean “and/or” unless explicitly indicated to refer to alternatives only or the alternatives are mutually exclusive, although the disclosure supports a definition that refers to only alternatives and “and/or.”
[0033] As used in this specification and claim(s), the words “comprising” (and any form of comprising, such as “comprise” and “comprises”), “having” (and any form of having, such as “have” and “has”), “including” (and any form of including, such as “includes” and “include”) or “containing” (and any form of containing, such as “contains” and “contain”) are inclusive or open-ended and do not exclude additional, unrecited elements or method steps.
[0034] Other objects, features and advantages of the present invention will become apparent from the following detailed description. It should be understood, however, that the detailed description and the examples, while indicating specific embodiments of the invention, are given by way of illustration only. Additionally, it is contemplated that changes and modifications within the spirit and scope of the invention will become apparent to those skilled in the art from this detailed description.
BRIEF DESCRIPTION OF THE DRAWINGS
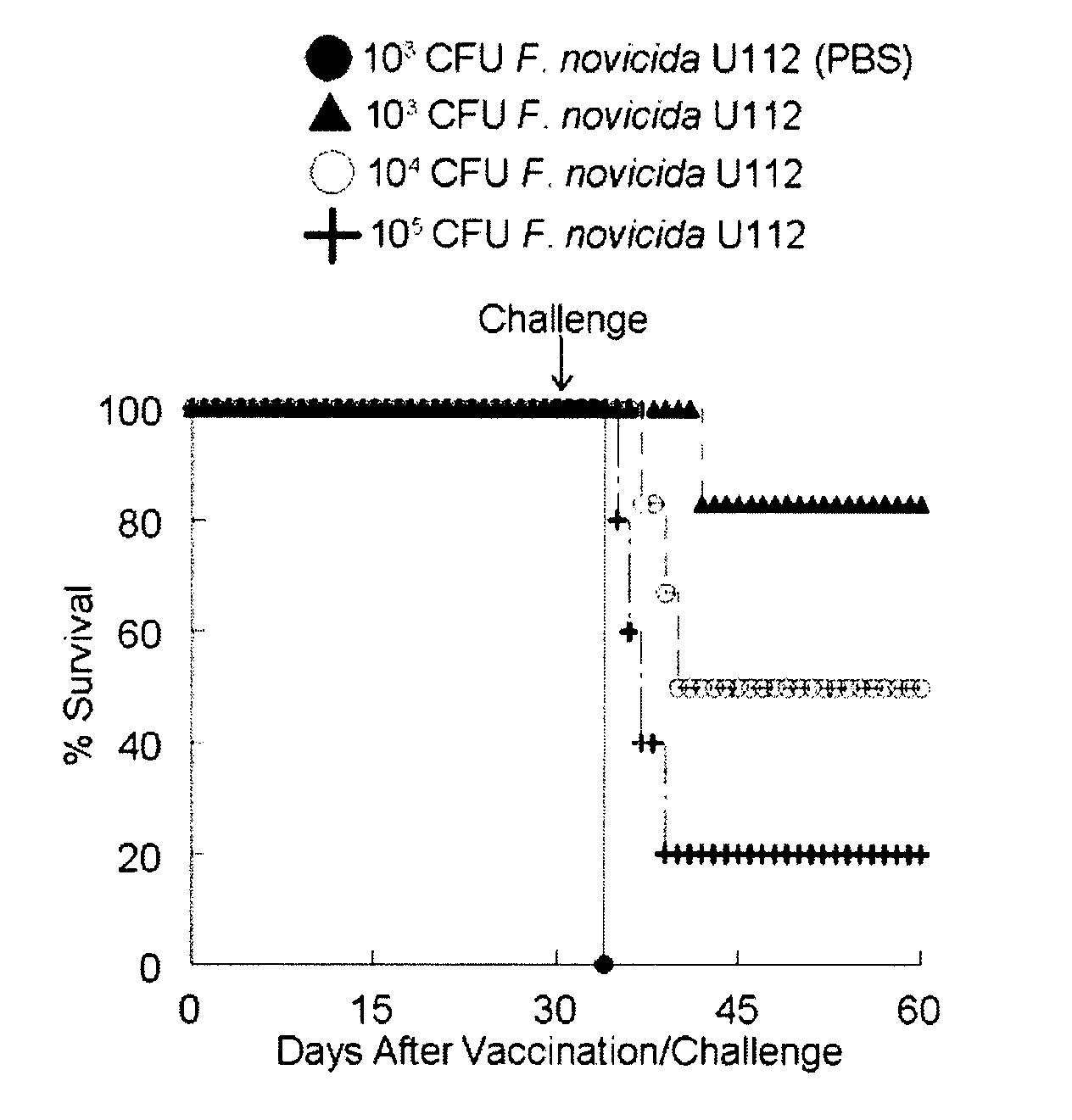
[0035]FIG. 1: Efficacy of intranasal vaccination with KKF24. BALB/c mice (6 mice/group) were anesthetized with 3% Isofluorane and vaccinated immediately i.n. with KKF24 (106 CFU) in 25 μl of sterile PBS. Unvaccinated mice received only PBS. All animals were challenged after 30 days with escalating inocula (100, 1000 and 10,000 LD50) of wild type F. tularensis subsp. novicida U112. All animals were monitored daily for survival. Differences in survival between KKF24 vaccinated and mock-vaccinated mice were significant at p<0.001. Results are representative of 2 independent experiments.
[0036]FIG. 2: Intranasal vaccination with KKF24 induces minimal pulmonary histopathological changes. Lungs were harvested from vaccinated animals, prepared for histological study and stained with H&E. (A) KKF24 primed lung day 3; (B) KKF24 primed lung day 60; (C) KKF24 primed and wild type challenged lung day 60; (D) PBS mock-treated and wild type challenged lung day 3; (E) PBS mock-treated animal. Magnification 10×. Results are representative of 2 independent experiments.
[0037]FIG. 3: Immunofluorescence staining of F. tularensis subsp. novicida following pulmonary challenge. Lungs were harvested from vaccinated animals and sections were stained with R-phycoerythrin conjugated rat anti-mouse CD11b (red) and anti F. novicida LPS monoclonal ab #8.2 (green). Nuclear staining (blue) was visualized with Bisbenzimide H 33258. (A) KKF24 primed lung day 3; (B) KKF24 primed lung day 60; (C) KKF24 primed and wild type challenged lung day 60; (D) PBS mock-treated and wild type challenged lung day 3; (E) PBS mock-treated animal. Magnification 20×. Results are representative of 2 independent experiments.
[0038]FIG. 4: Cytokine recall responses after vaccination with KKF24. BALB/c mice (3 mice/group) were anesthetized with 3% Isoflurane and vaccinated i.n. with KKF24 (106 CFU) in 25 μl of sterile PBS. On day 10, spleen and lymph node cells were tested for KKF24-induced IFN (A) and IL-12 (B) secretion by ELISA. Differences in IFN and IL-12 secretion between cells exposed to KKF24 and cells alone were significant at p<0.005. Results are representative of 3 independent experiments.
[0039]FIG. 5: Serum antibody profiles after vaccination with i.n. with KKF24. BALB/c mice were first anesthetized with 3% Isofluorane and primed i.n. with KKF24 (106 CFU) in 25 μl of sterile PBS. All animals were bled at day 30 and subsequently challenged with 100 LD50 of wild type F. tularensis subsp. novicida U 112. Surviving animals were bled on day 60 sera and were analyzed by isotype-specific ELISA using UV inactivated KKF24-coated microtiter plates. The results are reported as 50% end point titers. Differences in antibody binding between immune serum and normal mouse serum for total ab, IgG1 and IgG2a were significant at p<0.005. Results are representative of 3 independent experiments.
[0040]FIG. 6: IFN-dependent KKF24-mediated protection. BALB/c IFN−/− mice and IFN+/+ mice (6 mice/group) were anesthetized with 3% Isofluorane and vaccinated i.n. with KKF24 (106 CFU) in 25 μl of sterile PBS. Animals were challenged after 30 days with 50 LD50 (A) and 100 LD50 (B) of wild type F. tularensis subsp. novicida U112 respectively. All animals were monitored daily for survival. Differences in survival between vaccinated IFN+/+ mice and IFN−/− mice were significant at p<0.001. Results are representative of 2 independent experiments.
[0041]FIG. 7: Enhanced antibody-dependent phagocytic activity against F. tularensis subsp. novicida. F. tularensis subsp. novicida U112 was opsonized with varying concentrations of normal mouse serum (nms) or immune serum obtained from KKF24 vaccinated BALB/c mice. Phagocytosis was performed with the J774A.1 macrophage cell line (MOI of 1:1; bacteria to macrophage ratio). Cells were stained by anti-F. novicida LPS monoclonal ab #8.2 and anti-mouse CD11b and visualized by fluorescence microscopy. The percentage of macrophages containing bacteria was used as a measure of phagocytic activity. Results are shown as the mean percentage of macrophages containing fluorescent bacteria±SEM. 5% sera and nms: p<0.004; 10% sera and nms: p<0.005; 20% sera and nms: p<0.001. Results are representative of 2 independent experiments.
[0042]FIG. 8: Contribution of antibodies to KKF24-mediated protection. C57BL/6 μMT (B cell deficient) and C57BL/6 wild-type mice (6/group) were anesthetized with 3% Isoflurane and vaccinated i.n. with KKF24 (106 CFU) in 25 μl of sterile PBS. Animals were challenged after 30 days with 100 LD50 (A) of wild type F. tularensis subsp. novicida U 112. (B) Adoptive transfer of immune or normal serum to naïve C57BL/6 μMT animals. Immune serum was prepared from C57BL/6 mice vaccinated i.n. with KKF24. Normal serum was collected from unvaccinated C57BL/6 mice. Naïve C57BL/6 μMT animals (6/group) were injected i.p. with 200 μl of either pooled immune or normal serum (1:3 dilution) at −8 h before i.n. challenge with 100 LD50 of F. tularensis subsp. novicida. All animals were also injected with similar amounts of either immune or normal mouse serum at 24 h, 48 h and 72 h after bacterial challenge. Animals were monitored daily for morbidity and mortality. Results are representative of 2 independent experiments.
DESCRIPTION OF ILLUSTRATIVE EMBODIMENTS
[0043]F. tularensis can be classified into several subspecies, including those relevant to human disease: F. tularensis subsp. tularensis (type A) and F. tularensis subsp. holarctica (type B) (Titball et al., 2003). An additional subspecies, F. tularensis subsp. novicida, has low virulence for humans but shares a high degree of antigenic and genetic similarities to F. tularensis types A and B (Forsman et al., 1994), and maintains high virulence in mice (Lauriano et al., 2004; Pammit et al., 2004), thus making subsp. novicida infections of mice an attractive model for tularemia vaccine development.
[0044]F. tularensis subsp. tularensis is classified as one of the most infectious pathogenic bacteria because inhalation with only a few organisms will cause disease and significant mortality (Saslaw et al., 1961). F. tularensis also is considered a potential biological weapon and has been developed as a germ warfare agent by several government programs (Christopher et al., 1997; Dennis et al., 2001; Harris, 1992). In this regard, the respiratory tract and lungs are major portals of entry for inhalation exposure and serve as primary sites of infection before systemic spread.
[0045] Aerosol exposure to F. tularensis leads to high levels of morbidity and mortality, yet there currently is no tularemia vaccine approved for human usage in the U.S. Because F. tularensis is an intracellular pathogen, a live attenuated strain is a potentially effective means of vaccination. While LVS vaccination has been shown to provide protection against aerosol challenge with F. tularensis subsp. tularensis in mice and humans (Eigelsbach and Downs, 1961; Saslaw et al., 1961; Wu et al., 2005), the basis for attenuation of the LVS strain is unknown, thus bringing its safety for humans into question.
[0046] The inventors have discovered attenuated Francisella bacterium vaccines that overcome the deficiencies of previously known vaccines such as the LVS vaccine. The Francisella bacterium can include an alteration in the nucleic acid sequence encoding the mglA, iglA, iglB, iglC, and/or iglD genes of the bacterium. The IglA, iglB, IglC, and IglD genes are duplicated in the F. tularensis subsp. tularensis and F. tularensis subsp. holartica genomes.
[0047] As discussed below, the alteration can be, for example, a deletion, substitution, or insertion mutation in the mglA, iglA, iglB, iglC, and/or iglD genes of the bacterium. Additionally, the bacterium can be incorporated into pharmaceutical compositions that can be administered to a subject to induce an immune response. The immune response, in certain aspects, can be a protective or therapeutic immune response.
[0048] These and other aspects of the present invention are described in further non-limiting detail in the following sections.
[0000] A. iglC, iglD, iglA, iglB, and mglA
[0049] The iglC gene encodes a 23 kDa protein that is upregulated during intramacrophage growth in the Francisella bacterium. The nucleotide and amino acid sequences of iglC from Francisella tularensis subspec. novicida are described in SEQ ID NOS: 1 and 2 and can be found at gene bank accession numbers AY293579 and AAP58964 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of iglC from Francisella tularensis subspec. tularensis are described in SEQ ID NOS: 3 and 4 and can be found at gene bank accession numbers NC—006570, NC—006570, YP—170309, and YP—170617 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of iglC from Francisella tularensis subspec. holarctica are described in SEQ ID NOS: 5 and 6, respectively and can be found on the world wide web at theseed.uchigaco.edu/FIG/index.cgi (the contents of which are incorporated by reference). This gene has been shown to be important for intramacrophage survival and growth of subsp. novicida (Feldman et al., 2001; Gray et al., 2002). Moreover, iglC mutants of subsp. novicida are highly attenuated for virulence in mice and growth within amoebae (Golovliov et al., 2003; Lauriano et al., 2004). IglC is important for the inhibition of phagosome-lysosome fusion (Santic et al., 2005), escape from the phagosome (Lindgren et al., 2004; Santic et al., 2005) and induction of apoptosis in infected macrophages (Lai et al., 2004). IglC also may play a role in the downregulation of TLR-mediated signaling (Telepnev et al., 2003).
[0050] Similar to the iglC gene, the iglD gene encodes a protein that is essential for intramacrophage survival, escape from the phagosome, and induction of apoptosis (see Table 1 and 2 below). The nucleotide and amino acid sequences of iglD from Francisella tularensis subspec. novicida are described in SEQ ID NOS: 7 and 8 and can be found at gene bank accession numbers AY293579 and AAP58965 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of iglD from Francisella tularensis subspec. tularensis are described in SEQ ID NOS: 9 and 10 and can be found at gene bank accession numbers NC—006570, YP—170308, and YP—170616 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of iglD from Francisella tularensis subspec. holarctica are described in SEQ ID NOS: 11 and 12, respectively and can be found on the world wide web at theseed.uchigaco.edu/FIG/index.cgi (the contents of which are incorporated by reference).
[0051] The iglA and iglB genes encode proteins that appear to be essential for intramacrophage survival and virulence (see Table 1 and 2 below, and Gray et al., 2002). The nucleotide and amino acid sequences of iglA from Francisella tularensis subspec. novicida are described in SEQ ID NOS: 13 and 14 and can be found at gene bank accession numbers AY293579 and AAP58962 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of iglA from Francisella tularensis subspec. tularensis are described in SEQ ID NOS: 15 and 16 and can be found at gene bank accession numbers NC—006570, YP—170311, and YP—170619 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of iglA from Francisella tularensis subspec. holarctica are described in SEQ ID NOS: 17 and 18, respectively and can be found on the world wide web at theseed.uchigaco.edu/FIG/index.cgi (the contents of which are incorporated by reference). The nucleotide and amino acid sequences of iglB from Francisella tularensis subspec. novicida are described in SEQ ID NOS: 19 and 20 and can be found at gene bank accession numbers AY293579 and AAP58963 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of iglB from Francisella tularensis subspec. tularensis are described in SEQ ID NOS: 21 and 22 and can be found at gene bank accession numbers NC—006570, YP—170310, and YP—170618 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of iglB from Francisella tularensis subspec. holarctica are described in SEQ ID NOS: 23 and 24 and can be found on the world wide web at theseed.uchigaco.edu/FIG/index.cgi (the contents of which are incorporated by reference).
[0052] The mglA gene shares homology with SspA of Escherichia coli, which regulates stationary-phase gene transcription by interacting with RNA polymerase. mglA also plays a role in stimulating transcription of iglA, iglC and iglD. The nucleotide and amino acid sequences of mglA from Francisella tularensis subspec. novicida are described in SEQ ID NOS: 25 and 26 and can be found at gene bank accession numbers AF045772 and AAC29032 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of mglA from Francisella tularensis subspec. tularensis are described in SEQ ID NOS: 27 and 28 and can be found at gene bank accession numbers NC—006570 and YP—170231 (the contents of which are incorporated by reference), respectively. The nucleotide and amino acid sequences of mglA from Francisella tularensis subspec. holarctica are described in SEQ ID NOS: 29 and 30, respectively.
[0053] The complete nucleic acid sequence for the F. tularensis subsp. novicida pathogenicity island can be found at gene bank accession number AY293579, which is incorporated by reference. The complete nucleic acid sequence for the F. tularensis subsp. tularensis genome can be found at gene bank accession number NC—006570, which is incorporated by reference. The complete nucleic acid sequence for the F. tularensis subsp. holarctica genome can be found on the world wide web at theseed.uchigaco.edu/FIG/index.cgi (the contents of which are incorporated by reference).
[0000] B. Preparation of Attenuated Strains of Francisella Bacteria
[0054] In order for a modified Francisella strain to be effective in a vaccine formulation, the attenuation must be significant enough to prevent the pathogen from evoking severe clinical symptoms, but also insignificant enough to allow limited replication and growth of the bacteria in the recipient. The recipient is a subject needing protection or treatment from a disease caused by a virulent form of Francisella or other pathogenic microorganisms.
[0055] Attenuated Francisella bacteria can be made in several ways. For instance, methods such as subjecting wild-type Francisella bacteria having the mglA, iglA, iglB, iglC, and/or iglD genes to mutagenesis techniques known to those of skill in the art (Baron and Nano, 1998; Gray et al., 2002; Lauriano et al., 2003). Where employed, mutagenesis will be accomplished by a variety of standard, mutagenic procedures. Mutation is the process whereby changes occur in the quantity or structure of an organism. Mutation can involve modification of the nucleotide sequence of a single gene, blocks of genes or whole chromosomes. Changes in single genes may be the consequence of point mutations which involve the removal, addition, or substitution of a single nucleotide base within a DNA sequence (Cooley et al. 1988), or they may be the consequence of changes involving the insertion or deletion of large numbers of nucleotides. The mutation may act through affecting transcription or translation of the gene or its mRNA, or the mutation may affect the polypeptide gene product itself in such a way as to render it inactive.
[0056] In certain embodiments, attenuation of a Francisella Bacteria is carried out by deletion of a portion of the coding region of the mglA, iglA, iglB, iglC, and/or iglD genes. A deletion mutation can reduce the risk that the mutant will revert to a virulent state. For example, some, most (e.g., half or more), or virtually all of the coding region may be deleted (e.g., about 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 25, 30, 35, 40, 45, 50, 55, 60, 70, 80, 90, to about 100% of the gene). Alternatively, the mutation may be an insertion or deletion of even a single nucleotide that causes a frame shift in the open reading frame, which in turn may cause premature termination of the encoded polypeptide or expression of a completely inactive polypeptide. Mutations can also be generated through insertion of foreign gene sequences, e.g., the insertion of a gene encoding antibiotic resistance.
[0057] Deletion mutants can be constructed using any of a number of techniques that are known to those of skill in the art. In one non-limiting example, a strategy using counter selectable markers can be employed which has commonly been utilized to delete genes in many bacteria (Reyrat et al., 1998). In this technique, a double selection strategy is often employed wherein a plasmid is constructed encoding both a selectable and counter selectable marker, with flanking DNA sequences derived from both sides of the desired deletion. The selectable marker is used to select for bacteria in which the plasmid has integrated into the genome in the appropriate location and manner. The counter selecteable marker is used to select for the very small percentage of bacteria that have spontaneously eliminated the integrated plasmid. A fraction of these bacteria will then contain only the desired deletion with no other foreign DNA present.
[0058] In another technique, the cre/lox system is used for site specific recombination of DNA. Alternatively, site specific recombination can be achieved using the FLP recombinase techniques (Datsenko and Wanner, 2000). The system consists of 34 base pair lox sequences that are recognized by the bacterial cre recombinase gene. If the lox sites are present in the DNA in an appropriate orientation, DNA flanked by the lox sites will be excised by the cre recombinase, resulting in the deletion of all sequences except for one remaining copy of the lox sequence. Using standard recombination techniques, it is possible to delete the targeted gene of interest in the Francisella genome and to replace it with a selectable marker (e.g., a gene coding for kanamycin resistance) that is flanked by the lox sites. Transient expression (by electroporation of a suicide plasmid containing the cre gene under control of a promoter that functions in Francisella of the cre recombinase should result in efficient elimination of the lox flanked marker. This process would result in a mutant containing the desired deletion mutation and one copy of the lox sequences.
[0059] Another approach includes directly replacing a desired deleted sequence in the Francisella genome with a marker gene, such as green fluorescent protein (GFP), β-galactosidase, or luciferase. In this technique, DNA segments flanking a desired deletion are prepared by PCR and cloned into a suicide (non-replicating) vector for Francisella. An expression cassette, containing a promoter active in Francisella and the appropriate marker gene, is cloned between the flanking sequences. The plasmid is introduced into wild-type Francisella. Bacteria that incorporate and express the marker gene (probably at a very low frequency) are isolated and examined for the appropriate recombination event (i.e., replacement of the wild type gene with the marker gene).
[0060] Mutations can also be induced following exposure to chemical or physical mutagens. Such mutation-inducing agents include ionizing radiations, ultraviolet light, and a diverse array of chemical such as alkylating agents and polycyclic aromatic hydrocarbons all of which are capable of interacting either directly or indirectly (generally following some metabolic biotransformations) with nucleic acids. For instance, benzo[a]pyrene, N-acetoxy-2-acetyl aminofluorene and aflotoxin B1 cause GC to TA transversions in bacteria and mammalian cells. Benzo[a]pyrene also can produce base substitutions such as AT to TA. N-nitroso compounds produce GC to AT transitions. Alkylation of the O4 position of thymine induced by exposure to n-nitrosoureas results in TA to CG transitions. The DNA lesions induced by such environmental agents may lead to modifications of base sequence when the affected DNA is replicated or repaired and thus to a mutation.
[0061] Random mutations in the mglA, iglA, iglB, iglC, and/or iglD genes of a Francisella Bacterium can also be introduced using error prone PCR (Cadwell and Joyce, 1992). The rate of mutagenesis may be increased by performing PCR in multiple tubes with dilutions of templates. Alternatively, random mutations can be introduced by fragmentation and reassembly techniques (See U.S. Pat. No. 5,380,721). The method comprises obtaining polynucleotide library members, pooling and fragmenting the polynucleotides, and reforming fragments therefrom, performing PCR amplification, thereby homologously recombining the fragments to form a shuffled pool of recombined polynucleotides.
[0062] Site-directed mutagenesis can also be used to introduce mutations in the mglA, iglA, iglB, iglC, and/or iglD genes of a Francisella Bacterium (See, e.g., U.S. Pat. Nos. 5,220,007; 5,284,760; 5,354,670; 5,366,878; 5,389,514; 5,635,377; and 5,789,166). The technique provides for the preparation and testing of sequence variants by introducing one or more nucleotide sequence changes into a selected DNA.
[0063] Another aspect of the invention involves the construction of attenuated Francisella bacteria of the present invention that additionally comprise a polynucleotide sequence encoding a heterologous polypeptide. For example, for Francisella, a “heterologous” polypeptide would be a non-Francisella polypeptide not normally expressed by Francisella bacteria. Such attenuated bacteria can be used in methods for delivering the heterologous polypeptide or DNA. For example, Francisella could be engineered to lyse upon entry into the cytoplasm of a eukaryotic host cell without causing significant damage, thereby becoming a vector for the introduction of plasmid DNA into the cell. Suitable heterologous polypeptides include immunogenic antigens from other infectious agents (including gram-negative bacteria, gram-positive bacteria and viruses) that induce a protective immune response in the recipients, and expression of the polypeptide antigen by the mutant bacteria in the vaccine causes the recipient to be immunized against the antigen. Other heterologous polypeptides that can be introduced using the Francisella include immunomodulatory molecules e.g., cytokines or “performance” proteins such as growth hormone, GRH, and GDF-8.
[0000] C. Vaccine Preparations and Routes of Administration
[0064] 1. Vaccine Preparation
[0065] Once produced, synthesized, and/or purified, the attenuated Francisella Bacterium can be prepared as a vaccine for administration to a subject. The preparation of a vaccine is generally well understood in the art, as exemplified by U.S. Pat. Nos. 4,608,251, 4,601,903, 4,599,231, 4,599,230, and 4,596,792. Such methods may be used to prepare a vaccine comprising an immunogenic composition comprising at least one Francisella Bacterium as active ingredient(s), in light of the present disclosure. In certain embodiments, the compositions of the present invention are prepared to be pharmacologically acceptable vaccines.
[0066] Pharmaceutical vaccine compositions of the present invention comprise an effective amount of one or more Francisella Bacterium or additional agent dissolved or dispersed in a pharmaceutically acceptable carrier. The phrases “pharmaceutical or pharmacologically acceptable” refers to molecular entities and compositions that do not produce an adverse, allergic or other untoward reaction when administered to an animal, such as, for example, a human, as appropriate. The preparation of a pharmaceutical composition that contains at least one Francisella Bacterium or additional active ingredient will be known to those of skill in the art in light of the present disclosure, as exemplified by Remington's Pharmaceutical Sciences, 18th Ed. Mack Printing Company, 1990. Moreover, for animal (e.g., human) administration, it will be understood that preparations should meet sterility, pyrogenicity, general safety and purity standards as required by FDA Office of Biological Standards.
[0067] As used herein, “pharmaceutically acceptable carrier” includes any and all solvents, dispersion media, coatings, surfactants, antioxidants, preservatives (e.g., antibacterial agents, antifungal agents), isotonic agents, absorption delaying agents, salts, preservatives, drugs, drug stabilizers, binders, excipients, disintegration agents, lubricants, sweetening agents, flavoring agents, dyes, such like materials and combinations thereof, as would be known to one of ordinary skill in the art (see, e.g., Remington's 1990). The vaccines of the present invention may comprise different types of carriers depending on whether it is to be administered in solid, liquid or aerosol form, and whether it needs to be sterile for such routes of administration as injection. Except insofar as any conventional carrier is incompatible with the active ingredient, its use in the therapeutic or pharmaceutical compositions is contemplated.
[0068] The actual dosage amount of a vaccine composition of the present invention can be determined by physical and physiological factors such as body weight, severity of condition, the type of disease being treated, previous or concurrent therapeutic interventions, idiopathy of the patient and on the route of administration. The practitioner responsible for administration will, in any event, determine the concentration of active ingredient(s) in a composition and appropriate dose(s) for the individual subject.
[0069] In certain non-limiting embodiments, pharmaceutical compositions may comprise, for example, at least about 0.1% of an active ingredient. In other embodiments, the active ingredient may comprise between about 2% to about 75% of the weight of the unit, or between about 25% to about 60%, for example, and any range derivable therein. In other non-limiting examples, a dose may also comprise from about 1 microgram/kg/body weight, about 5 microgram/kg/body weight, about 10 microgram/kg/body weight, about 50 microgram/kg/body weight, about 100 microgram/kg/body weight, about 200 microgram/kg/body weight, about 350 microgram/kg/body weight, about 500 microgram/kg/body weight, about 1 milligram/kg/body weight, about 5 milligram/kg/body weight, about 10 milligram/kg/body weight, about 50 milligram/kg/body weight, about 100 milligram/kg/body weight, about 200 milligram/kg/body weight, about 350 milligram/kg/body weight, about 500 milligram/kg/body weight, to about 1000 mg/kg/body weight or more per administration, and any range derivable therein. In non-limiting examples of a derivable range from the numbers listed herein, a range of about 5 mg/kg/body weight to about 100 mg/kg/body weight, about 5 microgram/kg/body weight to about 500 milligram/kg/body weight, etc., can be administered, based on the numbers described above.
[0070] A person of ordinary skill will recognize that the vaccine compositions of the present invention can include at least about 0.0001% to about 0.001%, 0.001% to about 0.01%, 0.01% to about 0.1%, 0.2%, 0.3%, 0.4%, 0.5%, 0.6%, 0.7%, 0.8%, 0.9%, 1.0%, 1.1%, 1.2%, 1.3%, 1.4%, 1.5%, 1.6%, 1.7%, 1.8%, 1.9%, 2.0%, 2.1%, 2.2%, 2.3%, 2.4%, 2.5%, 2.6%, 2.7%, 2.8%, 2.9%, 3.0%, 3.1%, 3.2%, 3.3%, 3.4%, 3.5%, 3.6%, 3.7%, 3.8%, 3.9%, 4.0%, 4.1%, 4.2%, 4.3%, 4.4%, 4.5%, 4.6%, 4.7%, 4.8%, 4.9%, 5.0%, 5.1%, 5.2%, 5.3%, 5.4%, 5.5%, 5.6%, 5.7%, 5.8%, 5.9%, 6.0%, 6.1%, 6.2%, 6.3%, 6.4%, 6.5%, 6.6%, 6.7%, 6.8%, 6.9%, 7.0%, 7.1%, 7.2%, 7.3%, 7.4%, 7.5%, 7.6%, 7.7%, 7.8%, 7.9%, 8.0%, 8.1%, 8.2%, 8.3%, 8.4%, 8.5%, 8.6%, 8.7%, 8.8%, 8.9%, 9.0%, 9.1%, 9.2%, 9.3%, 9.4%, 9.5%, 9.6%, 9.7%, 9.8%, 9.9%, 10%, 11%, 12%, 13%, 14%, 15%, 16%, 17%, 18%, 19%, 20%, 21%, 22%, 23%, 24%, 25%, 26%, 27%, 28%, 29%, 30%, 35%, 40%, 45%, 50%, 60%, 65%, 70%, 75%, 80%, 85%, 90%, 95%, or 99% or any range derivable therein, of an attenuated Francisella Bacterium or other ingredients (e.g., additional vaccine components, pharmaceutical excipients, etc.) In non-limiting aspects, the percentage can be calculated by weight or volume of the total composition.
[0071] The vaccine component(s) may be formulated into a composition in a free base, neutral or salt form. Pharmaceutically acceptable salts, include the acid addition salts, e.g., those formed with the free amino groups of a proteinaceous composition, or which are formed with inorganic acids such as, for example, hydrochloric or phosphoric acids, or such organic acids as acetic, oxalic, tartaric or mandelic acid. Salts formed with the free carboxyl groups can also be derived from inorganic bases such as, for example, sodium, potassium, ammonium, calcium or ferric hydroxides; or such organic bases as isopropylamine, trimethylamine, histidine or procaine.
[0072] In embodiments where the composition is in a liquid form, a carrier can be a solvent or dispersion medium comprising but not limited to, water, ethanol, polyol (e.g., glycerol, propylene glycol, liquid polyethylene glycol, etc), lipids (e.g., triglycerides, vegetable oils, liposomes) and combinations thereof. The proper fluidity can be maintained, for example, by the use of a coating, such as lecithin; by the maintenance of the required particle size by dispersion in carriers such as, for example, liquid polyol or lipids; by the use of surfactants such as, for example, hydroxypropylcellulose; or combinations thereof. In many cases, one can include isotonic agents, such as, for example, sugars, sodium chloride or combinations thereof.
[0073] In other embodiments, one may use eye drops, nasal solutions or sprays, aerosols or inhalants in the present invention. Such compositions are generally designed to be compatible with the target tissue type. In a non-limiting example, nasal solutions are usually aqueous solutions designed to be administered to the nasal passages in drops or sprays. Nasal solutions are prepared so that they are similar in many respects to nasal secretions, so that normal ciliary action is maintained.
[0074] In certain embodiments the vaccine component(s) are prepared for administration by such routes as oral ingestion. In these embodiments, the composition may comprise, for example, solutions, suspensions, emulsions, tablets, pills, capsules (e.g., hard or soft shelled gelatin capsules), sustained release formulations, buccal compositions, troches, elixirs, suspensions, syrups, wafers, or combinations thereof. Oral compositions may be incorporated directly with the food of the diet. Carriers for oral administration comprise inert diluents, assimilable edible carriers or combinations thereof. In other aspects of the invention, the oral composition may be prepared as a syrup or elixir, and may comprise, for example, at least one active agent, a sweetening agent, a preservative, a flavoring agent, a dye, a preservative, or combinations thereof.
[0075] Sterile injectable solutions are prepared by incorporating the active compounds in the required amount in the appropriate solvent with various of the other ingredients enumerated above, as required, followed by filter sterilization. Generally, dispersions are prepared by incorporating the various sterilized active ingredients into a sterile vehicle which contains the basic dispersion medium and/or the other ingredients. In the case of sterile powders for the preparation of sterile injectable solutions, suspensions or emulsion, certain methods of preparation are vacuum-drying or freeze-drying techniques which yield a powder of the active ingredient plus any additional desired ingredient from a previously filter-sterilized liquid medium thereof. The liquid medium should be suitably buffered if necessary and the liquid diluent first rendered isotonic prior to injection with sufficient saline or glucose. The preparation of highly concentrated compositions for direct injection is also contemplated, where the use of DMSO as solvent is envisioned to result in extremely rapid penetration, delivering high concentrations of the active agents to a small area.
[0076] 2. Routes of Administration
[0077] The present invention can be administered intravenously, intradermally, intraarterially, intraperitoneally, intralesionally, intracranially, intraarticularly, intraprostaticaly, intrapleurally, intratracheally, intranasally, intravitreally, intravaginally, intrauterinely, intrarectally, intrathecally, topically, intratumorally, intramuscularly, intraperitoneally, subcutaneously, subconjunctival, intravesicularlly, mucosally, intrapericardially, intraumbilically, intraocularally, orally, topically, locally, inhalation (e.g. aerosol inhalation), injection, infusion, continuous infusion, localized perfusion bathing target cells directly, via a catheter, via a lavage, in cremes, in lipid compositions (e.g., liposomes), or by other method or any combination of the forgoing as would be known to one of ordinary skill in the art (Remington's, 1990).
[0000] D. Monitoring Immunogenic Response and Protective Immunity
[0078] An “immunologically protective amount” of the attenuated mutant bacteria is an amount effective to induce an immunogenic response in the recipient that is adequate to prevent or ameliorate signs or symptoms of disease, including adverse health effects or complications thereof, caused by infection with wild type Francisella bacteria. Either humoral immunity or cell-mediated immunity or both may be induced. The immunogenic response of an animal to a vaccine composition may be evaluated, e.g., indirectly through measurement of antibody titers, lymphocyte proliferation assays, or directly through monitoring signs and symptoms after challenge with wild type strain. The protective immunity conferred by a vaccine can be evaluated by measuring, e.g., reduction in clinical signs such as mortality, morbidity, temperature number and % of days of diarrhea, milk production or yield, average daily weight gain, physical condition and overall health and performance of the subject.
[0000] E. Additional Vaccine Components
[0079] It is contemplated that a vaccine or immunogenic composition of the present invention can be combined with one or more additional components (e.g., components other than the attenuated Francisella bacteria of the present invention) to form a more effective vaccine. Non-limiting examples of additional components include, for example, one or more additional immunogens, immunomodulators, or adjuvants to stimulate an immune response to an immunogenic composition of the present invention and/or the additional component(s).
[0080] 1. Immunomodulators
[0081] It is contemplated that immunomodulators can be included in the vaccine to augment a cell's or a subject's response. Immunomodulators can be included as purified proteins, nucleic acids encoding immunomodulators, and/or cells that express immunomodulators in the vaccine composition. The following sections list non-limiting examples of immunomodulators that are of interest, and it is contemplated that various combinations of immunomodulators may be used in certain embodiments.
[0083] Interleukins, cytokines, nucleic acids encoding interleukins or cytokines, and/or cells expressing such compounds are contemplated as possible vaccine components. Interleukins and cytokines, include but are not limited to interleukin 1 (IL-1), IL-2, IL-3, IL-4, IL-5, IL-6, IL-7, IL-8, IL-9, IL-10, IL-11, IL-12, IL-13, IL-14, IL-15, IL-18, -interferon, -interferon, γ-interferon, angiostatin, thrombospondin, endostatin, GM-CSF, G-CSF, M-CSF, METH-1, METH-2, tumor necrosis factor, TGF, LT and combinations thereof.
[0085] Chemokines, nucleic acids that encode for chemokines, and/or cells that express such also may be used as vaccine components. Chemokines generally act as chemoattractants to recruit immune effector cells to the site of chemokine expression. It may be advantageous to express a particular chemokine coding sequence in combination with, for example, a cytokine coding sequence, to enhance the recruitment of other immune system components to the site of treatment. Such chemokines include, for example, RANTES, MCAF, MIP1-alpha, MIP1-Beta, IP-10 and combinations thereof. The skilled artisan will recognize that certain cytokines are also known to have chemoattractant effects and could also be classified under the term chemokines.
[0086] iii. Immunogenic Carrier Proteins
[0087] In certain embodiments, a vaccine or immunogenic composition may be chemically coupled to a carrier or recombinantly expressed with a immunogenic carrier peptide or polypeptide (e.g., an antigen-carrier fusion peptide or polypeptide) to enhance an immune reaction. Exemplary immunogenic carrier amino acid sequences include hepatitis B surface antigen, keyhole limpet hemocyanin (KLH) and bovine serum albumin (BSA). Other albumins such as ovalbumin, mouse serum albumin or rabbit serum albumin also can be used as immunogenic carrier proteins. Means for conjugating a polypeptide or peptide to a immunogenic carrier protein are well known in the art and include, for example, glutaraldehyde, m-maleimidobenzoyl-N-hydroxysuccinimide ester, carbodiimide and bis-biazotized benzidine.
[0088] iv. Biological Response Modifiers
[0089] It may be desirable to co-administer biologic response modifiers (BRM), which have been shown to upregulate T cell immunity or downregulate suppressor cell activity. Such BRMs include, but are not limited to, cimetidine (CIM; 1200 mg/d) (Smith/Kline, Pa.); low-dose cyclophosphamide (CYP; 300 mg/m2) (Johnson/Mead, N.J.), or a gene encoding a protein involved in one or more immune helper functions, such as B-7.
[0091] Immunization protocols have used adjuvants to stimulate responses for many years, and as such adjuvants are well known to one of ordinary skill in the art. Some adjuvants affect the way in which immunogens are presented. For example, the immune response is increased when protein immunogens are precipitated by alum. Emulsification of immunogens also prolongs the duration of immunogen presentation.
[0092] In one aspect, an adjuvant effect is achieved by use of an agent, such as alum, used in about 0.05 to about 0.1% solution in phosphate buffered saline. Alternatively, the immunogen is made as an admixture with synthetic polymers of sugars (Carbopol®) used as an about 0.25% solution. Adjuvant effect may also be made by aggregation of the immunogen in the vaccine by heat treatment with temperatures ranging between about 70° to about 101° C. for a 30-second to 2-minute period. Aggregation by reactivating with pepsin-treated (Fab) antibodies to albumin, mixture with bacterial cell(s) such as C. parvum or an endotoxin or lipopolysaccharide components of Gram-negative bacteria, emulsion in physiologically acceptable oil vehicles, such as mannide mono-oleate (Aracel A) or emulsion with a 20% solution of a perfluorocarbon (Fluosol-DA®) used as a block substitute, also may be employed.
[0093] Some adjuvants, for example, certain organic molecules obtained from bacteria, act on the host rather than on the immunogen. An example is muramyl dipeptide (N-acetylmuramyl-L-alanyl-D-isoglutamine [MDP]), a bacterial peptidoglycan. Derivatives of muramyl dipeptide, such as the amino acid derivative threonyl-MDP, and the fatty acid derivative MTPPE, are also contemplated. The effects of MDP, as with most adjuvants, are not fully understood. MDP stimulates macrophages but also appears to stimulate B cells directly. The effects of adjuvants, therefore, are not immunogen-specific. If they are administered together with a purified immunogen, however, they can be used to selectively promote the response to the immunogen.
[0094] U.S. Pat. No. 4,950,645 describes a lipophilic disaccharide-tripeptide derivative of muramyl dipeptide which is described for use in artificial liposomes formed from phosphatidyl choline and phosphatidyl glycerol. It is thought to be effective in activating human monocytes and destroying tumor cells, but is non-toxic in generally high doses. The compounds of U.S. Pat. No. 4,950,645 and PCT Patent Application WO 91/16347, are contemplated for use with cellular carriers and other embodiments of the present invention.
[0095] Adjuvants have been used experimentally to promote a generalized increase in immunity against unknown immunogens (e.g., U.S. Pat. No. 4,877,611). In certain embodiments, hemocyanins and hemoerythrins may also be used in the invention. The use of hemocyanin from keyhole limpet (KLH) is used in certain embodiments, although other molluscan and arthropod hemocyanins and hemoerythrins can be employed.
[0096] Various polysaccharide adjuvants may also be used. For example, the effect of various pneumococcal polysaccharide adjuvants on the antibody response of mice has been described (Yin et al., 1989). The doses that produce optimal responses, or that otherwise do not produce suppression, should be employed as indicated (Yin et al., 1989). Polyamine varieties of polysaccharides can be used, such as chitin and chitosan, including deacetylated chitin.
[0097] Another adjuvant contemplated for use in the present invention is BCG. BCG (bacillus Calmette-Guerin, an attenuated strain of Mycobacterium) and BCG-cell wall skeleton (CWS) may also be used as adjuvants in the invention, with or without trehalose dimycolate. Trehalose dimycolate may be used itself. Trehalose dimycolate administration has been shown to correlate with augmented resistance to influenza virus infection in mice (Azuma et al., 1988). Trehalose dimycolate may be prepared as described in U.S. Pat. No. 4,579,945. BCG is an important clinical tool because of its immunostimulatory properties. BCG acts to stimulate the reticulo-endothelial system, activates natural killer cells and increases proliferation of hematopoietic stem cells. Cell wall extracts of BCG have proven to have excellent immune adjuvant activity. Molecular genetic tools and methods for mycobacteria have provided the means to introduce foreign genes into BCG (Jacobs et al., 1987; Snapper et al., 1988; Husson et al., 1990; Martin et al., 1990).
[0098] Amphipathic and surface active agents, e.g., saponin and derivatives such as QS21 (Cambridge Biotech), form yet another group of adjuvants for use with the immunogens of the present invention. Nonionic block copolymer surfactants (Rabinovich et al., 1994; Hunter et al., 1991) may also be employed. Oligonucleotides are another useful group of adjuvants (Yamamoto et al., 1988). Quil A and lentinen are other adjuvants that may be used in certain embodiments of the present invention.
[0099] One group of adjuvants for use in the invention are the detoxified endotoxins, such as the refined detoxified endotoxin of U.S. Pat. No. 4,866,034. These refined detoxified endotoxins are effective in producing adjuvant responses in mammals. Of course, the detoxified endotoxins may be combined with other adjuvants to prepare multi-adjuvant-incorporated cells. For example, combination of detoxified endotoxins with trehalose dimycolate is particularly contemplated, as described in U.S. Pat. No. 4,435,386. Combinations of detoxified endotoxins with trehalose dimycolate and endotoxic glycolipids is also contemplated (U.S. Pat. No. 4,505,899), as is combination of detoxified endotoxins with cell wall skeleton (CWS) or CWS and trehalose dimycolate, as described in U.S. Pat. Nos. 4,436,727, 4,436,728 and 4,505,900. Combinations of just CWS and trehalose dimycolate, without detoxified endotoxins, is also envisioned to be useful, as described in U.S. Pat. No. 4,520,019.
[0100] In other embodiments, the present invention contemplates that a variety of adjuvants may be employed in the membranes of cells, resulting in an improved immunogenic composition. The only requirement is, generally, that the adjuvant be capable of incorporation into, physical association with, or conjugation to, the cell membrane of the cell in question. Those of skill in the art will know the different kinds of adjuvants that can be conjugated to cellular vaccines in accordance with this invention and these include alkyl lysophospholipids (ALP); BCG; and biotin (including biotinylated derivatives) among others. Certain adjuvants particularly contemplated for use are the teichoic acids from Gram negative cells. These include the lipoteichoic acids (LTA), ribitol teichoic acids (RTA) and glycerol teichoic acid (GTA). Active forms of their synthetic counterparts may also be employed in connection with the invention (Takada et al., 1995a).
[0101] Various adjuvants, even those that are not commonly used in humans, may still be employed in animals, where, for example, one desires to raise antibodies or to subsequently obtain activated T cells. The toxicity or other adverse effects that may result from either the adjuvant or the cells, e.g., as may occur using non-irradiated tumor cells, is irrelevant in such circumstances.
[0102] One group of adjuvants for use in some embodiments of the present invention are those that can be encoded by a nucleic acid (e.g., DNA or RNA). It is contemplated that such adjuvants may be encoded in a nucleic acid (e.g., an expression vector) encoding the immunogen, or in a separate vector or other construct. These nucleic acids encoding the adjuvants can be delivered directly, such as for example with lipids or liposomes.
[0000] F. Vaccine Component Purification
[0103] A vaccine component may be isolated and/or purified from the chemical synthesis reagents, cell or cellular components. Purification can be accomplished by any appropriate technique that is described in the specification or known to those of skill in the art (e.g., Sambrook et al., 1987). There is no general requirement that a vaccine or immunogenic composition of the present invention or other vaccine component always be provided in their most purified state. Indeed, it is contemplated that a less substantially purified vaccine component, which is nonetheless enriched in the desired compound, relative to the natural state, will have utility in certain embodiments.
[0104] The present invention also provides purified and substantially purified vaccines or vaccine components. The term “purified vaccine component” as used herein, is intended to refer to at least one vaccine component wherein the component is purified to any degree relative to its naturally-obtainable state, e.g., relative to its purity within a cellular extract or reagents of chemical synthesis.
[0105] Where the term “substantially purified” is used, this will refer to a composition in which the specific compound forms the major component of the composition, such as constituting about 50% of the compounds in the composition or more. In certain aspects, a substantially purified vaccine component will constitute more than about 60%, about 70%, about 80%, about 90%, about 95%, about 99% or even more of the compounds in the composition.
[0106] Various techniques suitable for use in chemical, biomolecule or biological purification, well known to those of skill in the art, may be applicable to preparation of a vaccine component of the present invention. These include, for example, precipitation with ammonium sulfate, PEG, antibodies and the like or by heat denaturation, followed by centrifugation; fractionation, chromatographic procedures, including but not limited to, partition chromatograph (e.g., paper chromatograph, thin-layer chromatograph (TLC), gas-liquid chromatography and gel chromatography) gas chromatography, high performance liquid chromatography, affinity chromatography, supercritical flow chromatography, ion exchange chromatography, gel filtration chromatography, reverse phase chromatography, hydroxylapatite chromatography, lectin affinity chromatography; isoelectric focusing and gel electrophoresis (see for example, Sambrook et al. 1989; and Freifelder, Physical Biochemistry, Second Edition, pages 238-246).
[0000] G. Antibody Generation
[0107] In certain embodiments, isolated antibodies to the vaccine or immunogenic compositions of the present invention are contemplated as useful for purification, diagnostic and therapeutic applications. Monoclonal antibodies (MAbs) are recognized to have certain advantages, e.g., reproducibility and large-scale production, and their use is generally used. MAbs may be readily prepared through use of well-known techniques, such as those exemplified in U.S. Pat. No. 4,196,265.
[0108] In certain diagnostic or vaccine component purification aspects, an antibody specific to one or more vaccine components may be used. Non-limiting examples of such immunodetection methods include enzyme linked immunosorbent assay (ELISA), radioimmunoassay (RIA), immunoradiometric assay, fluoroimmunoassay, chemiluminescent assay, bioluminescent assay, and Western blot, to mention a few. The steps of various useful immunodetection methods have been described in the scientific literature, such as, e.g., Doolittle and Ben-Zeev, 1999; Gulbis and Galand, 1993; De Jager et al., 1993; and Nakamura et al., 1987. Often, the antibody may be conjugated with an imaging agent to enhance detection of a vaccine component ligand bound to the antibody, as would be known to one of ordinary skill in the art. Many appropriate imaging agents are known in the art, as are methods for their attachment to antibodies (see, for e.g., U.S. Pat. Nos. 5,021,236; 4,938,948; and 4,472,509).
[0109] In general, the detection of immunocomplex formation is well known in the art and may be achieved through the application of numerous approaches. These methods are generally based upon the detection of a label or marker, such as radioactive, fluorescent, biological and enzymatic tags. U.S. patents concerning the use of such labels include U.S. Pat. Nos. 3,817,837; 3,850,752; 3,939,350; 3,996,345; 4,277,437; 4,275,149 and 4,366,241. Of course, one may find additional advantages through the use of a secondary binding ligand such as a second antibody and/or a biotin/avidin ligand binding arrangement, as is known in the art.
[0000] H. Combination Therapy
[0110] In order to increase the effectiveness of the immunogenic and vaccine compositions of the present invention (“present compositions”), it may be desirable to combine the present compositions with other agents or vaccine components and methods effective in treating or preventing Francisella infection. The additional agents or vaccine components that can be used in the context of the present invention include such agents or vaccine components known to those of skill in the art (including those disclosed in other sections of the present specification).
[0111] This process can involve administering the combination of the present compositions with another agent(s) or vaccine component to the subject at the same time, for example, using a single composition or pharmacological formulation that includes both agents, or using two distinct compositions or formulations given at the same time, wherein one composition includes the compositions of the present invention which is administered before, during, or after the additional agent or vaccine component. The exact schedule of treatment with the present compositions and the second agent or vaccine component is determined in large part by the pharmacokinetic or pharmacodynamic properties of compositions being administered.
[0112] In embodiments where the present compositions and the additional agents or vaccine components are administered separately to the subject, one may wish that a significant period of time did not expire between the time of each delivery, such that the second agent or vaccine component and the present compositions would be able to exert an advantageously combined effect on the subject. In such instances, it is contemplated that one may administer to the subject with both modalities within about 12-24 h of each other or within about 6-12 h of each other. In some situations, it may be desirable to extend the time period for treatment significantly, however, where several days (2, 3, 4, 5, 6 or 7) to several weeks (1, 2, 3, 4, 5, 6, 7 or 8) lapse between the respective administrations.
[0113] Various combinations may be employed, such as where the present compositions is “A” and the second agent or vaccine component is “B”:
| A/B/A B/A/B B/B/A A/A/B A/B/B B/A/A A/B/B/B B/A/B/B |
| B/B/B/A B/B/A/B A/A/B/B A/B/A/B A/B/B/A B/B/A/A |
| B/A/B/A B/A/A/B A/A/A/B B/A/A/A A/B/A/A A/A/B/A |
|
I. Kits
[0114] In still further embodiments, the present invention concerns kits for use with the vaccination methods described above. Immunogenic compositions comprising attenuated Francisella bacteria may be provided in a kit. Such kits may be used to provide immunogens, vaccine components or vaccine preparations for vaccination in a ready to use and storable container.
[0115] The container of the kits can generally include at least one vial, test tube, flask, bottle, syringe and/or other container, into which at least one immunogenic composition, antibody, vaccine component or vaccine may be placed and/or suitably aliquoted. The kits of the present invention may include a means for containing vaccine components, vaccines or any other reagent containers in close confinement for commercial sale. Such containers may include injection and/or blow-molded plastic containers into which the desired vials are retained.
EXAMPLES
[0116] The following examples are included to demonstrate certain non-limiting aspects of the invention. It should be appreciated by those of skill in the art that the techniques disclosed in the examples which follow represent techniques discovered by the inventor to function well in the practice of the invention. However, those of skill in the art should, in light of the present disclosure, appreciate that many changes can be made in the specific embodiments which are disclosed and still obtain a like or similar result without departing from the spirit and scope of the invention.
Example 1
Experimental Set-Up and Procedures
[0117] Bacteria. F. tularensis subsp. novicida U112 was provided by Dr. Francis Nano (University of Victoria, Canada). Construction of the isogenic strain KKF24 (F. tularensis subsp. novicida ΔiglC::ermC (ΔiglC::ermC, see SEQ ID NO:31)) has been described (Lauriano et al., 2003). Strains were grown at 37° C. in Typticase Soy broth (TSB) supplemented with 0.1% cysteine.
[0118] Mice. Six to eight-week old female BALB/c mice were obtained from the National Cancer Institute (Bethesda, Md.). BALB/c IFN-γ−/− mice and C57BL/6 μMT (B cell deficient) mice and wild-type animals were obtained from the Jackson Laboratories (Bar Harbor, Me.). All animal care and experimental procedures were performed in compliance with the Institutional Animal Care and Use Committee (IACUC) guidelines.
[0119] Intranasal immunization and pulmonary challenge. Mice were first anesthetized with 3% Isofluorane using a rodent anesthesia system (Harvard Apparatus, Holliston, Mass.) (Murthy et al., 2004; Pammit et al., 2004), then inoculated intranasally with 106 CFU of KKF24 in 25 μl of PBS. Mock-vaccinated animals were treated with PBS alone. All animals were then challenged 4 weeks later, i.n. as described above, with escalating CFU (100 LD50-10,000LD50) of U112 [the LD50 of U112 administered i.n. has been calculated as 10 CFU (Lauriano et al., 2004)]. The actual CFU administered in each experiment was determined by serial dilution of inocula and plating on TSA supplemented with 0.1% cysteine. Animals were monitored daily for morbidity and mortality. Sera were prepared by collection of blood from the orbital plexus.
[0120] Spleen and lymph node cell culture for cytokine profiles. Spleens and cervical lymph nodes were collected from mice 10 days following i.n. vaccination with 106 CFU of KKF24 or PBS (mock-vaccinated animals). Single cell suspensions were prepared (1×106 cells/well for spleen cells and 2×105 cells/well for lymph node cells) and cultured in DMEM supplemented with 10% (v/v) FCS (Mediatech, Fairfax, Va.) ±105 CFU of UV-inactivated KKF24 for 72 h. Cells also were cultured with the unrelated antigen hen egg lysozyme (HEL). Culture supernatants were harvested for IFN-γ, IL-12 and IL-4 analysis by ELISA as described previously (Pammit et al., 2004). Lymph nodes and spleens from vaccinated mice were simultaneously evaluated for viable bacteria. No viable bacteria were recovered at 10 days post inoculation from the examined tissues.
[0121] Detection of antibody and isotype levels by ELISA. Microtiter plates were coated overnight with 106 CFU of UV-inactivated KKF24 in sodium bicarbonate buffer (pH 9.5), washed with PBS containing 0.3% Brij-35 (Sigma) and blocked for 1 h at room temperature with PBS containing 2% bovine serum albumin (BSA, EM Science Gibbstown, N.J.). Serial dilutions of serum were added to wells and incubated at room temperature for 2 h. The plates were then washed and incubated for an additional 1 h with goat anti-mouse total Ig, IgG1 and IgG2a conjugated to alkaline phosphatase (Southern Biotechnology Associates, Birmingham, Ala.). After incubation for 1 h, the plates were washed and p-nitrophenyl phosphate substrate was added for color development. Absorbance at 405 nm was measured using an ELISA microplate reader (Biotek Instruments, Winooski, Vt.). The reciprocal serum dilutions corresponding to 50% maximal binding were used to obtain titers. No binding of immune sera was observed when the plates were coated with the unrelated antigen HEL.
[0122] Opsonophagocytosis assays. To examine the opsonic potential of the immune sera, an opsonophagocytosis assay was established using chamber slides (Lab-Tek, Nunc, Naperville, Ill.) that were seeded overnight with 1×105 J774A.1 cells (macrophage cell line; American Type Culture Collection, Manassas, Va.) overnight. Wild-type F. tularensis subsp. novicida U112 (105 CFU) was incubated with varying concentrations of heat inactivated immune (collected 30 days after i.n. vaccination) or normal mouse serum in Eppendorf tubes for 30 min at 37° C. with end-over-end rotation. The opsonized bacteria were then incubated for an additional 1 h at 37° C. with the J774A.1 macrophages in the chamber slides. Following incubation, the solutions containing the bacteria were removed, and macrophages were incubated with DMEM plus 10 μg/ml of gentamicin to eliminate extracellular bacteria. The macrophages then were washed 3-times with PBS and fixed with 2% paraformaldehyde solution overnight at 4° C. The macrophages were subsequently washed, treated with 1% saponin (Sigma) for 30 min at room temperature, incubated with 3% BSA (EM Science), and subsequently stained for 1 h at 37 C with R-PE conjugated rat anti-mouse CD11b (BD Bioscience), F. novicida LPS monoclonal ab #8.2 conjugated to Alexa 488, and Bisbenzimide H 33258 (Sigma) for nuclear staining. Cells were washed and images were acquired using an Axiocam digital camera (Zeiss, Thornwood, N.Y.) connected to a Zeiss Axioskop 2 Plus research microscope. Random fields were imaged and the number of cells containing bacteria were counted. The percentage of macrophages containing fluorescent bacteria was used as a measure of phagocytic activity.
[0123] Adoptive transfer studies. Immune serum was prepared by collection from 10 C57BL/6 mice four weeks after i.n. vaccination with 106 CFU of KKF24. Normal mouse serum was prepared from unvaccinated animals. Naïve C57BL/6 βMT (B cell deficient) recipient mice were injected i.p. with 200 μl of a 1:3 dilution of pooled immune or normal serum at −8 h before i.n. challenge with 100 LD50 of F. tularensis subsp. novicida. All animals also were injected with similar amounts of either immune or normal mouse serum at 24 h, 48 h and 72 h after bacterial challenge. Animals were monitored daily for morbidity and mortality.
[0124] Histology and immunofluorescence staining. Lungs were removed 3 days and 60 days after primary immunization and embedded in optimal cutting temperature (OCT) resin and snap frozen. Serial horizontal cryosections of 5 μm were prepared and placed on silane coated-slides (VWR International, West Chester, Pa.). All slides were dried overnight and fixed in fresh acetone for 20 s at room temperature. Some sections also were fixed with formalin for 10 min and stained by hematoxylin and eosin (H&E). For immunofluorescent staining, slides were blocked with 3% BSA for 5 min, followed by incubation with 10% normal rat serum (Sigma) for 30 min. Tissue sections were subsequently incubated with R-phycoerythrin (R-PE) conjugated rat anti-mouse CD11b (BD Biosciences, San Diego, Calif.) for 40 min. Some sections also were stained with anti-F. tularensis subsp. novicida LPS monoclonal antibody #8.2 (ImmunoPrecise Antibodies Ltd, Victoria, Canada) conjugated to Alexa 488 (BD Biosciences). Sections were then washed and mounted using fluorsave reagent (Calbiochem, La Jolla, Calif.) containing Hoescht stain for nuclear staining. Images were acquired using an Axiocam digital camera (Zeiss, Thornwood, N.Y.) connected to a Zeiss Axioskop 2 Plus research microscope.
[0125] Statistical Analysis. Survival data were analyzed by the Mann-Whitney rank sum test and the antibody titers and cytokine analyses were evaluated by Student's t-test using the statistical software program SigmaStat. The data are presented as mean±standard deviation. The number of repetitions of each experiment is indicated in the figure legends. Each experiment was repeated at least twice.
Example 2
Intranasal Vaccination with F. tularensis Subsp. novicida ΔiglC is Highly Efficacious Against Intranasal Challenge with the Wildtype Strain
[0126] To directly assess the efficacy of F. tularensis subsp. novicida ΔiglC to function as a vaccine, BALB/c mice were vaccinated i.n. with 106 CFU of KKF24. Vaccinated mice exhibited no signs of morbidity at this dosage and were challenged 30 days later i.n. with escalating inocula of the wild-type F. tularensis subsp. novicida U112 strain. As shown in FIG. 1, vaccinated animals challenged with 103 CFU (100 LD50) of U112 were highly protected (82% survival) with minimal loss of body weight (data not shown). When the challenge inoculum was increased to 104 CFU (1000 LD50) of U112, the survival rate decreased to 50%. Increasing the challenge inoculum further to 105 CFU (10,000 LD50) of U112 resulted in 20% survival. There was no survival of any unvaccinated animals at the challenge doses tested, indicating that all three inocula (103, 104, and 105 CFU) of U112 were lethal doses, as expected.
[0127] Histological analyses were performed on vaccinated and challenged mice, as shown in FIG. 2. Lung sections from mice vaccinated i.n. with 106 CFU KKF24 three days (FIG. 2A) or 60 days (FIG. 2B) post vaccination revealed open air spaces with normal pulmonary architecture and no obvious evidence of histopathological changes, similar to mock (PBS) treated and unchallenged mice (2E). Lung tissue of vaccinated mice that were challenged i.n. with 103 CFU of the wildtype U112 strain 30 days following challenge (FIG. 2C) appeared similar to the lung tissue of vaccinated unchallenged mice (FIG. 2B). In contrast, the lungs of mice mock-vaccinated with PBS and then challenged with 103 CFU of the wildtype U112 strain displayed severe consolidation and polymorphonuclear cell infiltration 3 days after challenge (FIG. 2D).
[0128] In situ immunohistochemistry (FIG. 3) was performed on lung tissue from vaccinated and challenged mice with anti-CD11b (red; stains macrophages) and anti-F. tularensis subsp. novicida LPS (green; stains bacteria). Mice vaccinated i.n. with 106 CFU KKF24 had very few bacteria within the lung sections three (FIG. 3A) or 60 days (FIG. 3B) after vaccination and showed modest to no influx of macrophages, in comparison to PBS mock-treated and challenged mice (FIG. 3D). Mice vaccinated i.n. with KKF24, and then challenged i.n. with 103 CFU of the wildtype U112 strain had no detectable bacteria within the lungs at 30 days post-challenge (FIG. 3C), whereas, abundant macrophages and bacteria could be detected in the lungs of mock-vaccinated mice challenged i.n. with 103 CFU of the wildtype U112 strain as early as three days post challenge (FIG. 3D). As expected, there were few macrophages and no detectable bacteria in mock (PBS) treated and unchallenged mice (FIG. 3E). In addition, parallel lung tissues were also evaluated for bacterial loads. The mice vaccinated i.n. with KK24 exhibited no viable bacteria within the lungs 3 days post-inoculation, and no recoverable bacteria 60 days after immunization, which illustrates the high degree of attenuation of this strain. These results, utilizing subsp. novicida, show that a F. tularensis ΔiglC strain is a viable candidate for a live attenuated vaccine against pneumonic tularemia.
Example 3
Vaccination with F. tularensis Subsp. novicida ΔiglC Induces a Th1-Type Immune Response
[0129] The inventors examined whether vaccination with the KKF24 strain induces antigen-specific cell mediated responses. Mice were vaccinated with KKF24 (106 CFU), then 10 days later spleen and lymph node cells were tested for F. tularensis subsp. novicida-induced cytokine recall response. As shown in FIG. 4A, the draining cervical lymph node and spleen cells stimulated with UV-inactivated KKF24 induced an appreciable IFN-γ response in a dose-dependent manner in culture. Similarly, there was potent IL-12 secretion (FIG. 4B) from the stimulated cells upon i.n. vaccination with KKF24. There was negligible IL-4 induction in stimulated cultures (data not shown). Cells from mock-vaccinated (PBS) animals had no cytokine responses upon recall with KKF24. In addition, there was no recall response in cells from vaccinated animals to the unrelated control antigen HEL.
[0130] Sera from KKF24-vaccinated mice were analyzed for antibody profiles 30 days after initial vaccination, as well as 30 days following challenge with the wildtype U112 strain. Intranasal immunization with 106 CFU KKF24 induced a robust primary antibody response that included the induction of subsp. novicida-specific total, IgG1 and IgG2a antibodies (FIG. 5). Following i.n. challenge of vaccinated animals with 103 CFU of the wildtype strain, surviving animals displayed higher subsp. novicida-specific IgG2a antibody titers, than IgG1 titers. No binding of immune sera was observed with the unrelated antigen HEL. The antibodies induced were specific, and the antigenic determinants of F. tularensis subsp. novicida that stimulated the reactivity of the antibodies are currently under investigation. Collectively, the results demonstrate that i.n. vaccination with KKF24 induces a robust Th1-type cytokine and antibody response.
Example 4
IFN-γ and F. tularensis Subsp. novicida ΔiglC-Mediated Protection
[0131] To determine the contribution of IFN-γ in protection mediated by the ΔiglC strain, BALB/c IFN-γ−/− and IFN-γ-+/+ mice were immunized i.n. with 106 CFU of the F. tularensis subsp. novicida KKF24 strain. Notably, the vaccinated IFN-γ−/− mice all survived the infection with KKF24, with no overt symptoms of disease, indicating the highly attenuated nature of the ΔiglC strain. Vaccinated mice were challenged i.n. 30 days later with either 50 LD50 (500 CFU, FIG. 6A) or 100 LD50 (1000 CFU, FIG. 6B) of the wild-type F. tularensis subsp. novicida strain U112. It was found that all of the IFN-γ−/− vaccinated mice quickly succumbed within 4-5 days to the pulmonary challenge with the wild-type strain, whereas 100% of the IFN-γ+/+ mice were completely protected against both challenge doses. Mock-vaccinated (PBS) IFN-γ+/+ and IFN-γ−/− were highly susceptible to the lethal challenges. These results indicate that IFN-γ-dependent mechanisms play a pivotal role during vaccination with KKF24 in shaping the protective immune response against i.n. challenge with the wildtype strain.
Example 5
Antibodies Contribute to the Protection Conferred by i.n. Vaccination with F. tularensis Subsp. novicida ΔiglC
[0132] To test the functional ability of such antibodies to mediate phagocytic uptake of F. tularensis subsp. novicida, the inventors utilized a complement-independent opsonophagocytic assay using the J774A.1 murine macrophage cell line (FIG. 7). Sera prepared from mice vaccinated with KKF24 and collected at 30 days efficiently mediated phagocytosis of the wildtype F. tularensis subsp. novicida strain U112 in a concentration dependent manner, whereas normal mouse serum did not. Similar results were observed with primary bone marrow derived macrophages (data not shown).
[0133] To further elucidate the role of humoral immunity in protection, B cell deficient (μMT) and wild type mice were vaccinated with 106 CFU KKF24, then challenged 30 days later with 100 LD50 of the F. tularensis subsp. novicida wildtype strain U112. As shown in FIG. 8A, vaccinated B cell deficient mice were found to be highly susceptible (20% survival) to the lethal wildtype subsp. novicida challenge, compared to similarly vaccinated wild-type (80% survival) mice. These results demonstrate a role for B cells in the protective immune response of ΔiglC-vaccinated mice.
[0134] To determine whether antibodies could reconstitute the protection in B cell deficient animals, adoptive transfer studies using immune or normal serum were performed. Adoptive transfer of immune serum from KKF24-vaccinated mice to naive B cell deficient mice afforded significant protection (80% survival) against i.n. lethal challenge with 100 LD50 of the F. tularensis subsp. novicida wildtype strain U112 (FIG. 8B). In contrast, all the B cell deficient recipient mice receiving normal mouse serum succumbed (0% survival) to the challenge by day 6. These results indicate that antibodies contribute to the protection afforded by i.n. vaccination with F. tularensis subsp. novicida ΔiglC.
Example 6
i.n. Challenges of Mice with F. tularensis is a Reasonable Model for Human Pneumonic Tularemia
[0135] The inventors utilized i.n. challenges of mice with F. tularensis subsp. novicida as a model for human pneumonic tularemia. Subsp. novicida infections are a reasonable model for tularemia because subsp. novicida has an LD50 similar to the subsp. tularensis strain via the i.n. route in mice, and hallmarks of disease appear similar during infection caused by the two subspecies (Forsman et al., 1994; Lauriano et al., 2004; Pammit et al., 2004). Furthermore, subsp. novicida behaves similar to subsp. tularensis within human macrophages (Clemens et al., 2004; Santic et al., 2005), suggesting that the underlying pathogenic mechanism utilized by both subspecies is similar.
[0136] Protective efficacy of subsp. novicida ΔiglC (SEQ ID NO: 31), ΔiglA (SEQ ID NO: 32), ΔiglD (SEQ ID NO: 33), ΔmglA (SEQ ID NO: 34) strains against wildtype subsp. novicida challenge are illustrated in Tables 1 and 2.
|
|
| Virulence of F. tularensis subsp. novicida |
| mutants in BALB/c mice: |
| Strain | LD50 intranasal | LD50 intraperitoneal |
| |
| mglA | >3.1 × 106 | >2.3 × 104 |
| iglA | >5.2 × 107 | N.D. |
| iglC | >9.4 × 107 | >1.7 × 106 |
| iglD | >9.7 × 108 | >1.8 × 107 |
| |
[0137] |
|
| Efficacy of Intranasal Vaccination with |
| F. tularensis subsp. novicida mutants: |
| Intranasal | Intranasal WT | |
| Strain | inoculum (CFU) | challenge (CFU) | Survivors |
|
| None (PBS) | — | 1000 | 0/5 |
| mglA | 1.3 × 105 | 1000 | 1/5 |
| iglA | 5.2 × 107 | 1000 | 5/5 |
| iglC | 3.8 × 106 | 1000 | 5/5 |
| iglD | 9.7 × 108 | 1000 | 5/5 |
|
[0138] All of the compositions and/or methods disclosed and claimed in this specification can be made and executed without undue experimentation in light of the present disclosure. While the compositions and methods of this invention have been described in terms of certain embodiments, it will be apparent to those of skill in the art that variations may be applied to the compositions and/or methods and in the steps or in the sequence of steps of the method described herein without departing from the concept, spirit and scope of the invention. More specifically, it will be apparent that certain agents which are both chemically and physiologically related may be substituted for the agents described herein while the same or similar results would be achieved. All such similar substitutes and modifications apparent to those skilled in the art are deemed to be within the spirit, scope and concept of the invention as defined by the appended claims.
REFERENCES
[0139] The following references, to the extent that they provide exemplary procedural or other details supplementary to those set forth herein, are specifically incorporated herein by reference.
- U.S. Pat. No. 3,817,837
- U.S. Pat. No. 3,850,752
- U.S. Pat. No. 3,939,350
- U.S. Pat. No. 3,996,345
- U.S. Pat. No. 4,196,265.
- U.S. Pat. No. 4,275,149
- U.S. Pat. No. 4,277,437
- U.S. Pat. No. 4,366,241
- U.S. Pat. No. 4,435,386
- U.S. Pat. No. 4,472,509
- U.S. Pat. No. 4,596,792
- U.S. Pat. No. 4,599,230
- U.S. Pat. No. 4,599,231
- U.S. Pat. No. 4,601,903
- U.S. Pat. No. 4,608,251
- U.S. Pat. No. 4,866,034
- U.S. Pat. No. 4,877,611
- U.S. Pat. No. 4,938,948
- U.S. Pat. No. 4,950,645
- U.S. Pat. No. 5,021,236
- U.S. Pat. No. 5,220,007
- U.S. Pat. No. 5,284,760
- U.S. Pat. No. 5,354,670
- U.S. Pat. No. 5,366,878
- U.S. Pat. No. 5,380,721
- U.S. Pat. No. 5,389,514
- U.S. Pat. No. 5,635,377
- U.S. Pat. No. 5,789,166
- U.S. Pat. No. 4,436,727
- U.S. Pat. No. 4,436,728
- U.S. Pat. No. 4,505,899
- U.S. Pat. No. 4,505,900
- U.S. Pat. No. 4,520,019
- U.S. Pat. No. 4,579,945
- Azuma et al., Cell Immunol., 116(1):123-134, 1988.
- Baron and Nano, Mol. Microbiol., 29:247-259, 1998.
- Cadwell and Joyce, PCR Methods Appl., 2(1):28-33, 1992.
- Christopher et al., JAMA, 278:412-417, 1997.
- Clemens et al., Infect. Immun., 72:3204-3217, 2004.
- Cooley et al., Science, 239(4844):1121-1128, 1988.
- Datsenko and Wanner, PNAS, 97(12):6640-45, 2000.
- De Jager et al., Semin. Nucl. Med., 23(2):165-179, 1993.
- Dennis et al., JAMA, 285:2763-2773, 2001.
- Doolittle and Ben-Zeev, Methods Mol Biol, 109:215-237, 1999.
- Eigelsbach and Downs, J. Immunol., 87:415-424, 1961.
- Ellis et al., Clin. Microbiol. Rev., 15:631-646, 2002.
- Feldman et al., N. Engl. J. Med., 345:1601-1606, 2001.
- Forsman et al., Int. J. Syst. Bacteriol., 44:38-46, 1994.
- Forsman et al., Int. J. Syst. Bacteriol., 44:38-46, 1994.
- Freifelder, In: Physical Biochemistry Applications to Biochemistry and Molecular Biology, 2nd Ed. Wm. Freeman and Co., NY, 1982.
- Golovliov et al., FEMS Microbiol. Lett., 222:273-280, 2003.
- Gray et al., FEMS Microbiol. Lett. 215, 53-56, 2002.
- Gray et al., FEMS Microbiol. Lett., 215:53-56, 2002.
- Gulbis and Galand, Hum. Pathol., 24(12):1271-1285, 1993.
- Harris, Ann. N.Y. Acad. Sci., 666:21-52, 1992.
- Hunter et al., Vaccine, 9(4):250-256, 1991.
- Husson et al., J. Bacteriol., 172(2):519-524, 1990.
- Jacobs et al., Nature, 327(6122):532-535, 1987.
- Lai et al., Microb. Pathog., 37:225-230, 2004.
- Lauriano et al., FEMS Microbiol. Lett., 229:195-202, 2003.
- Lauriano et al., Proc. Natl. Acad. Sci. USA, 101:4246-4249, 2004.
- Lindgren et al., J. Med. Microbiol., 53:953-958, 2004.
- Martin et al., Nature, 345(6277):739-743, 1990.
- Murthy et al., Cell Immunol., 230:56-64, 2004.
- Nakamura et al., In: Handbook of Experimental Immunology (4th Ed.), Weir et al (Eds.), 1:27, Blackwell Scientific Publ., Oxford, 1987.
- Pammit et al., Antimicrob. Agents Chemother., 48:4513-4519, 2004.
- PCT Appln. WO 91/16347
- Rabinovich et al., Science, 265(5177):1401-1404, 1994.
- Remington's Pharmaceutical Sciences, 18th Ed. Mack Printing Company, pp. 1289-1329, 1990.
- Reyrat et al., Infection and Immunity, 66:4011-4017, 1998.
- Sambrook et al., In: Molecular cloning: a laboratory manual, 2nd Ed., Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y., 1987.
- Sambrook et al, In: Molecular cloning: a laboratory manual, 2nd Ed., Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y., 1989.
- Santic et al., Cell Microbiol., 7:957-967; 969-979, 2005.
- Saslaw et al., Arch. Intern Med., 107:134-146. 1961.
- Snapper et al., Proc. Natl. Acad. Sci. USA, 85(18):6987-6991, 1988.
- Takada et al., Infection and Immunity, 63(1):57-65, 1995a.
- Tarnvik, Rev. Infect. Dis., 11:440-451, 1989.
- Telepnev et al., Cell Microbiol., 5:41-51, 2003.
- Titball et al., Trends Microbiol., 11:118-123, 2003.
- Wu et al., Infect. Immun., 73:2644-2654, 2005.
- Yamamoto et al., Nature, 334(6182):494-498, 1988.
- Yin et al., J. Biol. Resp. Modif., 8:190-205, 1989.